Navigation auf uzh.ch
Navigation auf uzh.ch
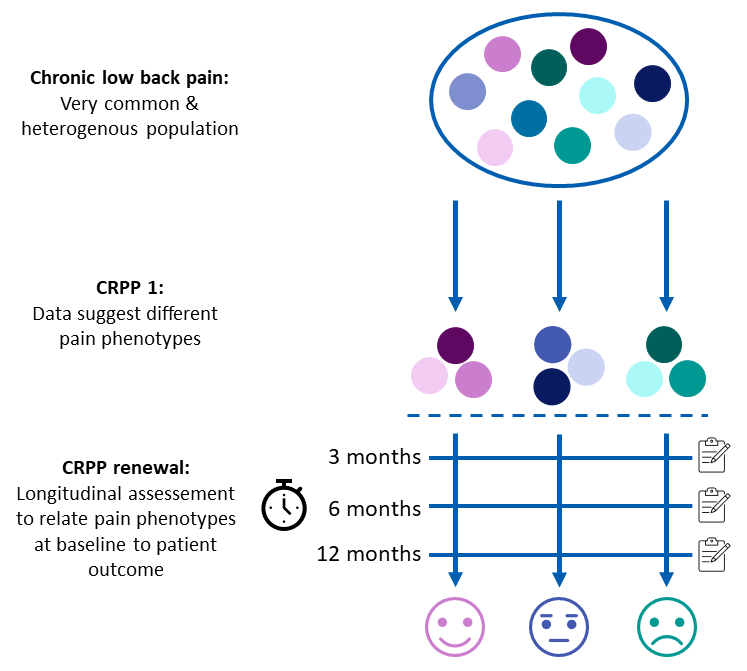
In the clinical part of WP3, we established a standardized psychophysical test battery to test spinal sensitization, descending pain modulation and the interaction of the two in the patients of the different cohorts (see WP1). Considering that the most painful body areas vary considerably across the cohorts, and therefore the testing sites, and that each cohort comes with its own set of challenges (e.g. reduced mobility in the SCI patients; necessity to test in prone position for the chronic low back pain (CLBP) patients), this is a major achievement. We also established a state-of-the-art brain imaging protocol, comprising resting state functional connectivity as well as an optimized magnetic resonance spectroscopy (MRS) protocol of the brain stem for in-depth investigation of patients with CLBP. In total, 136 patients (from all cohorts) and controls have completed the psychophysical test battery and 49 patients and controls the imaging protocol. Regarding CLBP, preliminary data analysis of suggests the existence of different pain phenotypes.
Renewal:
Based on the successful collaboration between WP1-3 in the first funding period, a CLBP core has been established for the renewal. The specific aims of this core include:
Aim 1: To identify a set of blood biomarkers that discriminates CLBP phenotypes.
We will investigate biological profiles/clusters across the CLBP patients who were studied in the first funding period and compare them to controls. The bioinformatic analysis will advance our understanding of cellular dysregulation in CLBP patients and of specific pathophysiological phenotypes. We will then integrate the data with the somatosensory, psychophysical, and clinical data to test if biological data support CLBP phenotype definition by somatosensory and psychophysical data.
Aim 2: To relate phenotype clusters at baseline to patient outcome.
The detailed cross-sectional assessment of patients with CLBP obtained in the first funding period is being complemented with longitudinal assessments using a reduced set of questionnaires and pain drawings at 3, 6 and 12 months. The dimensionality of baseline factors will be reduced using factor analysis and a machine learning approach will be used to identify the baseline factors that best predict clinical state in CLBP patients after 3, 6 and 12 months.
Aim 3: To determine the pathophysiological relevance of biological, psychophysical and psychological alterations via a longitudinal cohort of episodic CLBP patients.
To disentangle trait- and state-like alterations, patients with episodic CLBP will be studied during pain and pain-free periods and compared with healthy controls. The testing sessions will consist of a reduced battery of the cross-sectional CRPP assessment and will be based on the tests that best discriminated CLBP patients and controls during the first funding period.
The overarching goals of the CLBP core are to link pain phenotypes to pathophysiology and patient outcomes and to identify biomarkers that correlate with pain phenotypes. To this end, we will investigate which of the biological, psychophysical, psychological, and clinical alterations observed in CLBP patients are likely to be pathophysiologically relevant. We strive to combine these data to generate an integrated biopsychophysical model that identifies clinically meaningful CLBP phenotypes.